C Common Skin Concerns
Eczema and Psoriasis Management: A Comprehensive Review
By
Beauty Doctor MD September 26, 2023
Eczema (atopic dermatitis) and psoriasis are two chronic skin conditions that affect millions of individuals worldwide. While distinct in their etiology and presentation, both conditions share common features, such as chronic inflammation, itchiness, and a substantial impact on patients’ quality of life. This research article provides an in-depth review of the current understanding of eczema and psoriasis, their underlying mechanisms, diagnostic criteria, and comprehensive management strategies. We explore a range of treatments, including topical therapies, systemic medications, phototherapy, and emerging biologic agents, with a focus on individualized care and patient education.

Introduction
Eczema and psoriasis are dermatological conditions characterized by chronic inflammation and often debilitating symptoms. These conditions have distinct pathophysiological mechanisms, but they share common clinical features, including redness, itching, and the potential for flaring. Despite their prevalence, effective management remains a challenge, necessitating a multidimensional approach. This article aims to provide an up-to-date overview of eczema and psoriasis, encompassing their clinical presentation, pathogenesis, diagnostic criteria, and contemporary management strategies.
Eczema (Atopic Dermatitis)
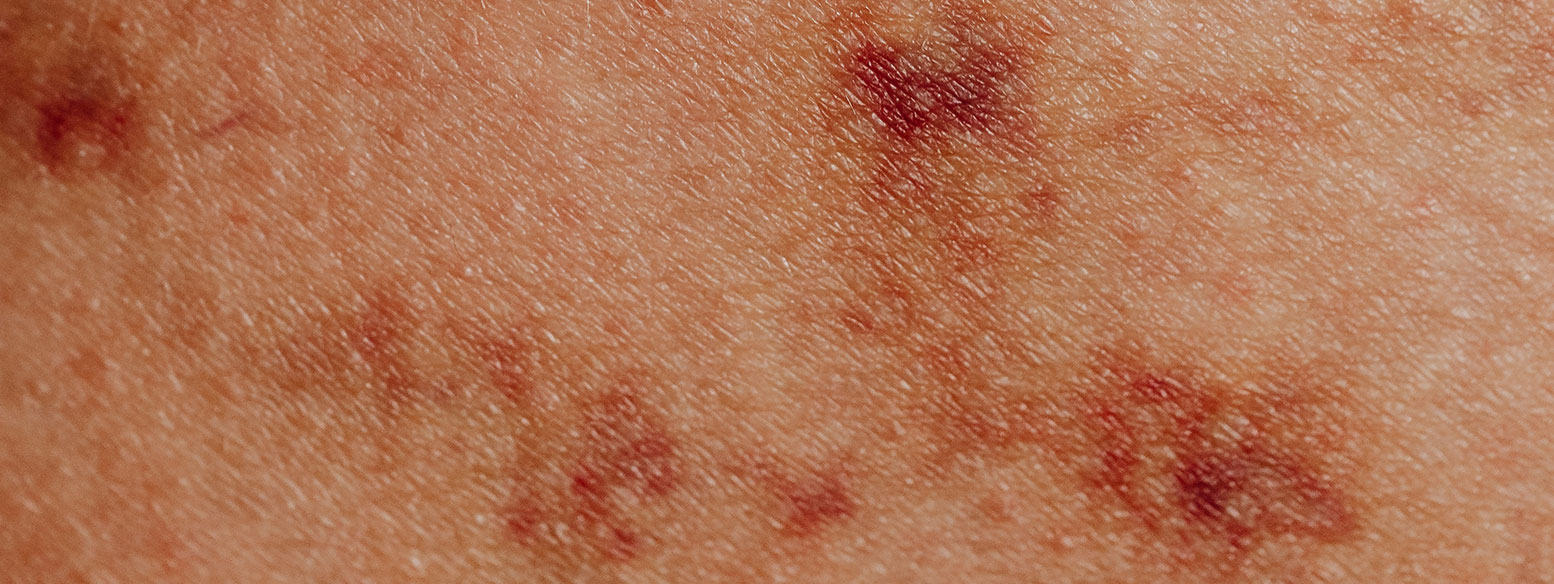
Clinical Presentation:
- Eczema typically presents as itchy, red, and inflamed skin.
- Lesions may range from dry, scaly patches to oozing, crusted areas.
- Common sites of involvement include the face, neck, elbows, and knees.
- Eczema often follows a relapsing-remitting course, with flares triggered by allergens, irritants, stress, or infections.
Pathogenesis:
- Eczema is multifactorial, with genetic, immune, and environmental factors contributing.
- Dysfunction of the skin barrier, driven by mutations in the filaggrin gene, is a key factor.
- Immune dysregulation, particularly an imbalance between Th1 and Th2 responses, plays a role.
- Allergens and irritants can exacerbate eczema by triggering immune responses.
Management:
- Topical Therapies: Emollients, topical corticosteroids, calcineurin inhibitors (e.g., tacrolimus), and crisaborole are commonly used.
- Systemic Treatments: In severe cases, systemic immunosuppressants like cyclosporine or dupilumab, a biologic agent, may be prescribed.
- Patient Education: Patients should be educated about trigger avoidance, proper skincare, and adherence to treatment plans.
Psoriasis
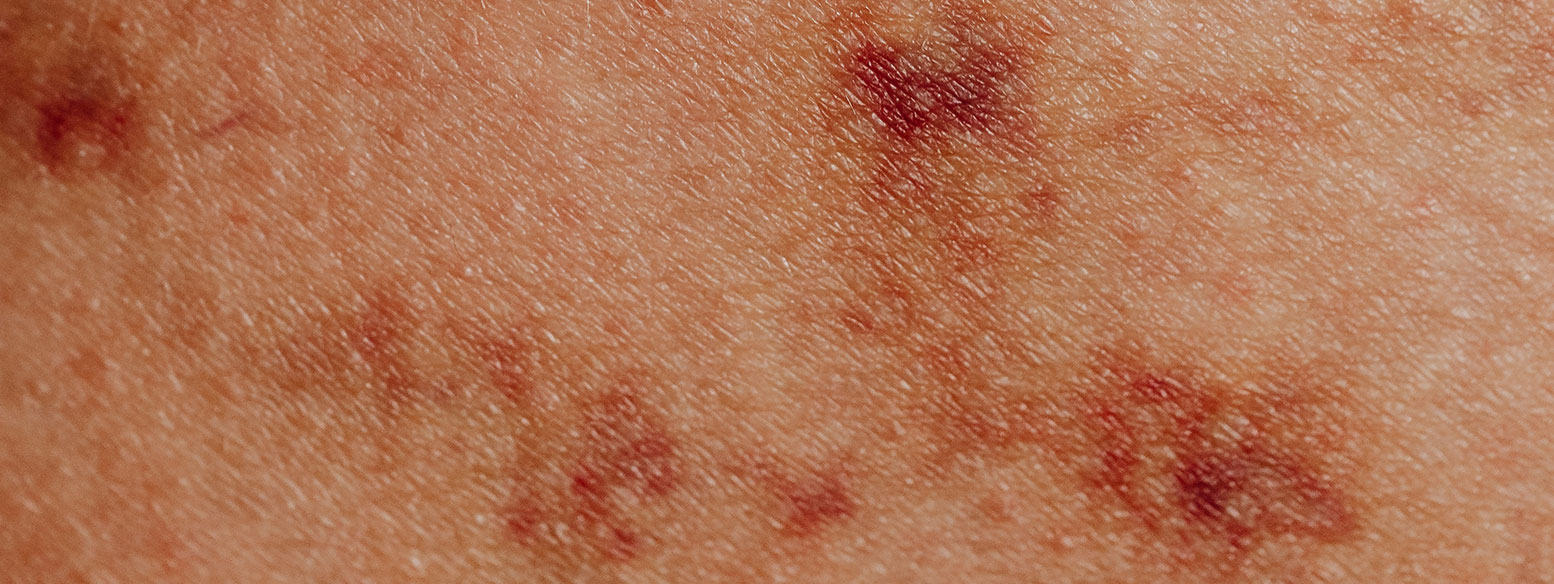
Clinical Presentation:
- Psoriasis is characterized by well-demarcated, red plaques covered with silvery-white scales.
- Lesions can occur anywhere but are often found on the elbows, knees, scalp, and lower back.
- Nail involvement (psoriatic nail dystrophy) and psoriatic arthritis are common extracutaneous manifestations.
Pathogenesis:
- Psoriasis is primarily driven by dysregulated immune responses, notably the activation of T cells and cytokine production.
- Genetic factors are significant, with several susceptibility genes identified.
- Environmental triggers, including trauma, infections, and stress, can provoke or exacerbate psoriasis.
Diagnostic Criteria:
- Diagnosis is clinical, based on characteristic skin lesions.
- The Psoriasis Area and Severity Index (PASI) quantifies disease severity.
- Histological examination may be necessary in atypical cases.
Management:
- Topical Therapies: Topical corticosteroids, vitamin D analogs (e.g., calcipotriol), and tar preparations are often used.
- Phototherapy: Narrowband UVB and psoralen plus UVA (PUVA) are effective for moderate psoriasis.
- Systemic Medications: Methotrexate, cyclosporine, and biologic agents (e.g., TNF-alpha inhibitors, IL-17 inhibitors) are options for severe cases.
- Lifestyle Management: Smoking cessation, alcohol moderation, and stress reduction can help manage psoriasis.
Comparative Analysis
- Eczema and psoriasis differ in their clinical appearance, with eczema featuring erythematous patches and psoriasis characterized by silvery scales.
- The underlying pathogenesis varies, with eczema involving skin barrier dysfunction and immune dysregulation, while psoriasis primarily stems from immune-mediated inflammation.
- Eczema commonly presents in childhood, while psoriasis typically occurs in adulthood.
- Both conditions benefit from topical therapies, but systemic treatments are more frequently used in psoriasis due to its chronicity and potential for severe manifestations.
Conclusion
Eczema and psoriasis are chronic dermatological conditions that pose significant challenges to patients and clinicians alike. Understanding their clinical presentation, pathogenesis, and management strategies is essential for providing effective care. While topical therapies play a crucial role, systemic treatments, including biologic agents, have revolutionized the management of psoriasis. Individualized treatment plans, patient education, and interdisciplinary collaboration can significantly improve the quality of life for individuals living with eczema and psoriasis. Future research may unveil novel therapeutic targets, further enhancing our ability to manage these complex skin conditions.